Report 23: Harmful Cytokines From Vaccinated Mothers Passed to Breastfed Infants – Report
Cytokines: A Cause for Concern
in MRNA-Vaccinated Pregnant and Nursing Women?
6/2/22
Cytokines and their effects have been in the headlines as long as Covid-19 has been with us. But what do we know about cytokines, and what do we know about the effects of cytokines on vaccinated pregnant and nursing women? How are cytokines related to mRNA vaccines and breast milk? This essay explores these questions and more.
Summary
Most important finding: Harmful cytokines from vaccinated mothers are passed to breastfed infants.
Key detail leading to finding: Increased levels of certain cytokines are shown to have deleterious effects in infants when passed from the mother’s milk during other (non-Covid-19) inflammatory events.
Events of concern:
1. Studies show that an imbalance in cytokines in breast milk may have severe consequences for the child, which in turn affects the child’s development. A permanent oversupply of cytokines may lead to an excessive stimulation/threat of the child’s immune system and subsequent onset of diseases. There is evidence of increased cytokines in breast milk during inflammatory processes and possible pathological effects of these higher cytokine levels on the newborn.
2. Studies show a link between infection and brain damage involving various mediators of inflammation, including cytokines, chemokines, and immune cells. These inflammatory mediators are also involved in brain-damaging processes that follow energy deprivation, as may occur with intrapartum asphyxia (deprivation of oxygen in a newborn).
3. Studies support the relationship between maternal inflammation with preterm birth and adverse neonatal outcomes. Mediators of inflammation, most notably proinflammatory cytokines, have been implicated as having an association with adverse neonatal outcomes.
4. Studies reveal a correlation with miscarriages and cytokine levels. In women at risk for spontaneous abortion, higher levels of proinflammatory cytokines were measured. It was concluded that changes in levels of cytokines could help predict and prevent the development of some of these complications.
5. A recent study found that immune responses to mRNA Covid-19 vaccination were present in most vaccinated women’s breast milk. Overall, among women who reported any side effects, the levels of one inflammatory cytokine were significantly higher in milk after vaccination than in milk provided before receiving the vaccine. While the study showed antibodies to SARS-COV2 being transferred via breast milk, they also found that levels of antibodies/cytokines correlated with vaccine side effects that mothers experienced.
Further investigation: Are increased cytokine levels following maternal vaccination with mRNA Covid-19 “vaccines”, that are noted to be associated with increases in maternal side effects, harmful to infants who are breastfed?
Scale of situation: For women who reported mRNA vaccine side effects, levels of one pro inflammatory cytokine increased by approximately 2.5-fold after the first dose and by more than 20-fold after the second dose.
Plain language explanation of key scientific term: Cytokines are small proteins released by immune cells to help regulate inflammatory and immune responses. Cytokines bind to a cell and signal to the cell how it needs to behave, which is why cytokines are often referred to as “messenger cells” because they carry a “message” with them as they travel through the body. For instance, they may give the message to increase inflammation or pain. Nearly every organ of the body contains cells that bind cytokines.
What are cytokines?
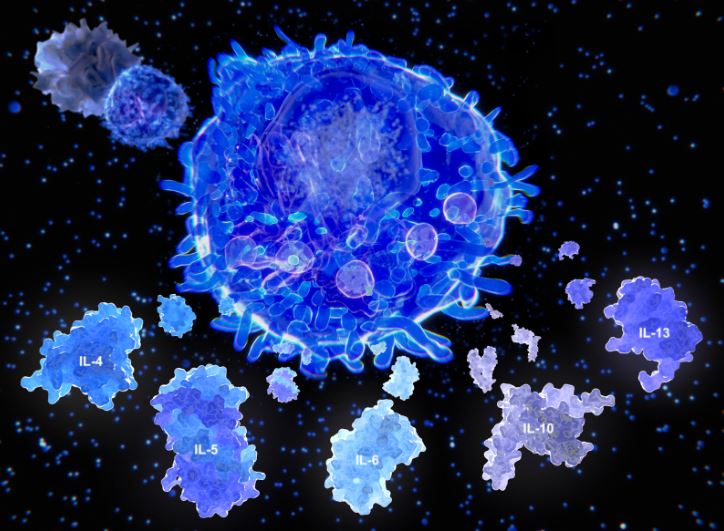
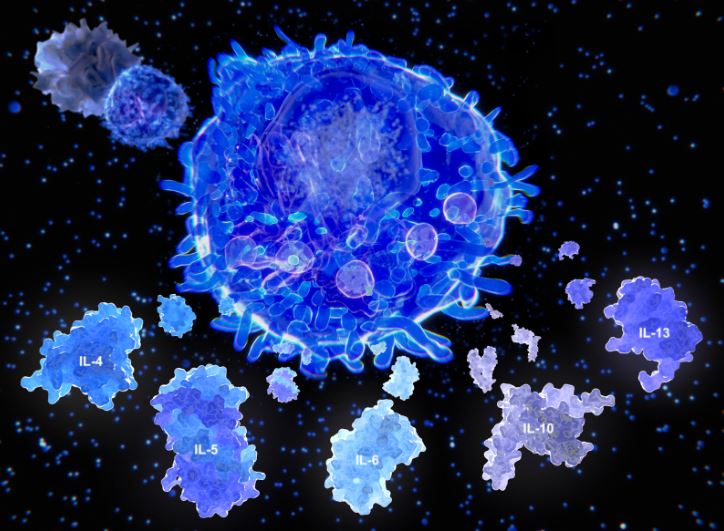
Cytokines are a large, diverse family of small proteins or glycoproteins that play an important role in regulating inflammatory and immune responses. According to Manoylov, M. K. (2020) these proteins are produced by many different immune cells, such as neutrophils, mast cells, macrophages, B-cells, and T-cells. Cytokines radiate out from immune cells and bind to specific receptors on other immune and non-immune cells. There the cytokines signal to the cell how it needs to behave, which is why cytokines are often referred to as “messenger cells” because they carry a “message” with them as they travel through the body. For instance, they may give the message to increase inflammation or pain. Nearly every organ of the body contains cells with cytokine receptors. Some of the various types of cytokines include: interleukins (IL 1-13), interferons (α, β, and γ), tumor necrosis factor (TNF), and transforming growth factor (TGF-β).
How do cytokines work?
When a pathogen or harmful substance enters the body, immune cells, cytokines, and organs work together to respond. The first cell to notice the pathogen directs all the other cells by creating and sending out messages (cytokines) to the rest of the cells or organs, which respond as directed. Because cytokines derived from the immune system (immunokines) are toxic to cells, they have been used against certain types of cancer. However, their clinical usefulness is limited due to their short half-life and their wide ranging and unpredictable side effects (Farlex Partner Medical Dictionary, 2012).
Cytokines play a broad role in helping the immune system respond to diseases and drugs which modulate their effect and have led to some beneficial therapies. Cytokines may be “good” when stimulating the immune system to fight a foreign pathogen, attack tumors, or reduce an immune response, such as inflammation in patients with multiple sclerosis. On the other hand, cytokines may be “bad” when their expression causes inflammatory diseases. Therapeutic modulation of cytokine expression can tell the “good” cytokines to generate or control the immune system and block the “bad” cytokines to prevent damaging inflammatory events. However, care must be exercised, as some antibody therapeutics can cause “ugly” cytokine release which can be deadly (Ramani, T., et al., 2015).
A severe immune reaction in which the body releases too many cytokines into the blood too quickly is known as a cytokine storm. A cytokine storm can occur as a result of infection, autoimmune condition, or other disease, or even after treatment with some types of immunotherapy (National Cancer Institute, 2022). This phenomenon was first described in 1993 as an uncontrolled inflammatory response caused by an excess number of cytokines being released, leading to over-activation of other immune cells like T-cells, macrophages, and natural killer cells. The uncontrolled activity of these cells can lead to tissue damage, organ dysfunction, and sometimes death. They were even thought to have been responsible for the high number of deaths in young people during the 1918 flu pandemic (de Wit, E., et al., 2018).
How do cytokines affect vaccinated pregnant and nursing women?
A literature review of “Inflammatory Breast Diseases during Lactation: Health Effects on the Newborn” was conducted in 2008 by Wöckel, A., et al. The review revealed that an imbalance in cytokines in breast milk may have severe consequences for the child, which in turn affects the child’s development. On one hand, a rise in cytokines in breast milk is useful to activate a mechanism of maternal self–defense against infectious processes and could also be useful in breastfed infants in order to activate or stimulate their immunity. However, it is possible that a permanent oversupply of cytokines leads to an excessive stimulation/threat of the child’s immune system and subsequent onset of diseases. The review further showed evidence of increased cytokines in breast milk during inflammatory processes and possible pathological effects of these higher cytokine levels on the newborn. Further study was recommended.
A study conducted by Dammann, O. and O’Shea, M. (2008) pointed out that evidence from epidemiological studies and experiments over more than 30 years in animals indicated that infection remote from the brain is a potential cause of cerebral white matter damage in human neonates. Since then, a large body of evidence suggests a link between infection and brain damage involving various mediators of inflammation, including cytokines, chemokines, and immune cells. These inflammatory mediators are also involved in brain-damaging processes that follow energy deprivation, as may occur with intrapartum asphyxia (deprivation of oxygen in a newborn). Equally as important is the role of cytokines in modulation of inflammation and repair after inflammation-related brain damage. The researchers suggest that strategies to reduce the frequency and extent of pre- and perinatal brain damage may derive from therapeutic interventions which either enhance the production or activity of certain “damage protectors” (e.g., anti-inflammatory cytokines) or inhibit the production or activity of specific “damage mediators” (e.g., inflammatory cytokines).
According to Pickler, R., et al. (2010), there is a growing body of literature supporting the relationship between maternal inflammation with preterm birth and adverse neonatal outcomes. Mediators of inflammation, most notably proinflammatory cytokines, have been implicated as having an association with adverse neonatal outcomes. Lyon, D., et al. (2010) conducted a systematic review of evidence from human studies for the association of levels of cytokines in the blood and preterm labor and adverse early fetal outcome. The most consistent finding was increased levels of proinflammatory cytokines; particularly interleukin (IL) 6, IL-1β, and tumor necrosis factor α (TNFα) were associated with preterm birth. A follow up review by Pickler, R., et al. (2010) of evidence from human studies on the association of cytokine levels in blood with two early adverse outcomes in preterm infants found early infection and increased risk of neurological damage. The review revealed that the proinflammatory cytokines most frequently linked with sepsis are in the IL-1 family as well as TNFα and IL-6. The proinflammatory cytokines most frequently associated with neurologic insult in the reviewed studies were IL-1β, IL-6, and IL-8. In all cases where IL-1β was studied, the levels were increased when there was a neurologic insult.
Other studies reveal a correlation with miscarriages and cytokine levels. Calleja-Agius, J., et al. (2011) conducted an observational study over a 1-year period of 94 Maltese women presenting with threatened abortion (TM) compared to 564 age–matched controls from the National Obstetric Information System (NOIS) of Malta. A pilot study was carried out with subgroups of 10 women with TM (n=10), non-pregnant women (n=12), normal pregnant controls (n=9), and women presenting with missed miscarriage (n=11), whose plasma levels of β-human chorionic gonadotropin (β-hCG), tumor necrosis factor α (TNFα), interferon γ (IFN γ), interleukin-6 (IL-6), interleukin-10 (IL-10), and TNF receptors 1 (R1) and 2 (R2) were measured. Of the 94 women with TM, 25 (26.6%) proceeded to complete miscarriage and had a significantly higher incidence of antepartum hemorrhage (p<0.005), preeclampsia (p<0.05), fetal growth restriction (p<0.05), premature labor (p<0.001), and retained placenta (p<0.005). Significantly (p<0.05) higher level of TNFα and lower levels of TNF R2 were found in the TM subgroup compared to non-pregnant controls. The ratio of TNFα/IL-10 was significantly (p<0.05) higher and the β-hCG levels were significantly lower (p<0.01) in missed miscarriages and non-pregnant subgroups than in TM and normal pregnant controls. The IFNγ/1L-10 and IFNγ/1L-6 were significantly (p<0.001) different between the four subgroups with the lowest level found in the TM group. No similar gradient was found for the TNFα/1L-6 ratio. Therefore, it was concluded that changes in levels of cytokines could help predict and prevent the development of some of these complications.
Recently, a study conducted at the University of Massachusetts by Narayanaswamy, V., et al. (2022) found that immune responses to mRNA Covid-19 vaccination were present in most women’s breast milk. The milk reportedly neutralized the spike protein in four (4) variants of concern, with the potential to confer passive immunity to the breastfed infant against SARS-COV2. The study measured levels of 10 key cytokines in milk of the 26 vaccinated lactating women who completed a questionnaire on side effects. The levels of IFNγ were significantly higher in milk provided after the first dose and after the second dose as compared to milk provided before receiving the vaccine. For women who reported side effects (n=13), compared with samples provided before vaccinations, the levels of IFNγ increased by approximately 2.5-fold in samples provided after the first dose and by more than 20-fold in samples provided after the second dose. Overall, among women who reported any side effects, the levels of IFNγ were significantly higher in milk after vaccination than in milk provided before receiving the vaccine. Among the women who reported no side effects after either the first or second dose (n=13), compared with samples provided before vaccination, the median levels of IFNγ increased by approximately 2-fold in samples provided after the first dose and by 3-fold in samples provided after the second dose. Levels of five of the seven other tested cytokines were comparable across the three time points; levels of the remaining two cytokines were not consistently detectable. While the study showed antibodies to SARS-COV2 being transferred via breast milk, they also found that levels of antibodies/cytokines correlated with vaccine side effects that mothers experienced.
The above University of Massachusetts study has since been heavily cited and reported on frequently in support of vaccinating women while pregnant and lactating. One of the researchers, K. F. Arcaro, was quoted as saying “women who did feel sick from the vaccine was [sic] associated with greater antibodies in the infant stool…so you might have felt badly, but that was a benefit for your infant” (Science Daily, 2022).
A cause for concern?
Clearly cytokines are a diverse group of protein molecules that can be both beneficial and harmful. Increased levels of certain cytokines are shown to have deleterious effects in infants when passed from the mother’s milk during other (non-Covid-19) inflammatory events. So why would increased cytokine levels following maternal vaccination with mRNA Covid-19 “vaccines,” that are also noted to be associated with increases in maternal side effects, be any less harmful or cause for concern?
References:
Calleja-Agius J, Schembri-Wismayer P, Calleja N, Brincat M, Spiteri D. Gynecol Endocrinol. 2011 Feb;27(2):121-7. doi: 10.3109/09513590.2010.487614. Epub 2010 May 26. PMID: 20500112. Obstetric outcome and cytokine levels in threatened miscarriage.
Dammann, O., O’Shea, T. M., Clinics in Perinatology. 2008 Dec; 35 (4): 643-663. Doi: 10.1016/j.clp. 2008.07.011. Cytokines and Perinatal Brain Damage.
de Wit, E., Siegers, J. Y., Cronin, J. M., Weatherman, S., van den Brand, J. M., Leijten, L. M., van Run, P., Begeman, L., van den Ham, H. J., Andeweg, A. C., Bushmaker, T., Scott, D. P., Saturday, G., Munster, V. J., Feldmann, H., van Riel, D. 2018. 1918 H1N1 Influenza Virus Replicates and Induces Proinflammatory Cytokine Responses in Extrarespiratory Tissues of Ferrets. The Journal of Infectious Diseases, 217(8), 1237–1246. https://doi.org/10.1093/infdis/jiy003
Farlex Partner Medical Dictionary. (2012). Cytokine. Retrieved May 24 2022 from https://medical-dictionary.thefreedictionary.com/cytokine
Lyon D., Cheng C.Y., Howland L., Rattican D., Jallo N., Pickler R., Brown L., McGrath J. Biological Research Nursing, 2010 Apr;11(4):371-76. doi: 10.1177/1099800409344620. Epub 2009 Dec 23. PMID: 20034950 Review. Integrated review of cytokines in maternal, cord, and newborn blood: Part I–associations with preterm birth. https://journals.sagepub.com/doi/10.1177/1099800409344620
Manoylov, M. K. LiveScience, 2020, Nov. 06.What are Cytokines?
https://www.livescience.com/what-are-cytokines.html
Narayanaswamy, V., Pentecost, B., Schoen, C., Alfandari, D., Schneider, S., Baker, R., Arcaro, K. 2022,Obstetrics & Gynecology, Neutralizing Antibodies and Cytokines in Breast Milk After Coronavirus Disease 2019 (COVID-19) mRNA Vaccination. https://journals.lww.com/greenjournal/pages/articleviewer.aspx?year=2022&issue=02000&article00006&type=Fulltext.
National Cancer Institute, 2022, medical terms. Cytokine Storm.
https://www.cancer.gov/publications/dictionaries/cancer-terms/def/cytokine-storm?redirect=true
Pickler R., Brown L., McGrath J., Lyon D., Rattican D., Cheng C.Y, Howland L., Jallo N.,
Biological Research Nursing 2010 Apr;11(4):377-86. doi: 10.1177/1099800409344619. Epub 2009 Dec 21.PMID: 20028689 Review. Integrated review of cytokines in maternal, cord and newborn blood: Part II-associations with early infection and increased risk of neurological damage in preterm infants. https://journals.sagepub.com/doi/pdf/10.1177/1099800409344619
Ramani, T., Auletta, C., Weinstock, C., Mounho-Zamora, B., Ryan , P., Salcedo, T., Bannish , G., May 26, 2015, International Journal of Toxicology, Cytokines: The Good, the Bad, and the Deadly. https://journals.sagepub.com/doi/full/10.1177/1091581815584918
Science Daily, January 10, 2022, University of Massachusetts Amherst, Vaccinated women pass COVID-19 antibodies to breastfeeding babies, study finds: Research detects SARS-CoV2 antibodies in infant stool. https://www.sciencedaily.com/releases/2022/01/220110103326.htm
Wöckel A., Abou-Dakn, M., Beggel, A., Arack, P., Mediators of Inflammation, vol. 2008, Article ID 298760, 2008.”Inflammatory Breast Diseases during Lactation: Health Effects on the Newborn—A Literature Review.” https://doi.org/10.1155/2008/298760



