“Covid-19 has laid bare the inequities in our health system. What are we going to do about it?”
Covid-19, which disproportionately affects people of color, continues to shine a light on the deep inequities ingrained in our society. Non-whites are more likely to be infected with the virus and suffer from severe illness than their white counterparts, according to data from the Centers for Disease Control and Prevention (CDC). Members of the American Indian and Alaska Native communities are 2.8 times more likely to be infected and 5.3 times more likely to be hospitalized than whites. Members of the Latinx community are 2.8 times more likely to be infected and 4.6 times more likely to be hospitalized compared to white people. Black people are 2.6 times more likely to be infected and 4.7 times more likely to be hospitalized.
Inequitable policies in our health, criminal justice, education, housing and employment systems, have created the conditions for Covid-19 to harm communities of color disproportionately. Many of these unjust systems continue to implement racist policies. The harmful impacts of these policies on health equity have led many local and state leaders to declare racism a public health crisis. Black and Latinx people are over-represented in jobs deemed essential during the coronavirus pandemic, and cannot work remotely. These jobs in transportation, local government, grocery stores, healthcare, and agriculture keep our society running, yet the workers are often poorly paid and not provided with adequate protective equipment. A study undertaken in Massachusetts of 104 grocery store workers, 61.5 percent of whom were non-white, found that twenty percent tested positive for the coronavirus. Many essential workers, and others not able to work from home during the pandemic, rely on public transportation, where risk of infection is increased, to get to work.
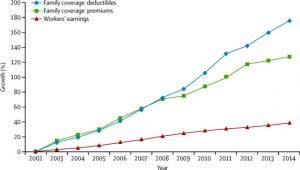
Structural inequities entrenched in our health system have resulted in higher rates of chronic diseases among the Black and Latinx populations in the US. These chronic diseases including diabetes, obesity, and hypertension put individuals with these conditions at a higher risk of developing severe illness from coronavirus infection. Non-whites are also uninsured or underinsured at higher rates than white people in the US, and may have to wait until they are very sick to seek treatment because of uncertainty about how they are going to afford care. When seeking medical care, Covid-19 outcomes among people of color may be worse due to under resourced and over-crowded hospitals often accessed by those in communities of color.
Centuries of racist housing, education, and economic policies have resulted in people of color in the United States disproportionately experiencing poverty. Living in crowded conditions, linked to low wages and unjust housing policies such as redlining, can facilitate the spread of the coronavirus and increase the risk of infection. In addition, environmental racism has resulted in higher levels of exposure to air pollution in Black and Latinx communities compared with white communities. A study conducted by researchers at Harvard found that individuals living in areas with high levels of air pollution before the pandemic were more likely to die from Covid-19.
Over-policing, harsh drug laws, and strict non-discretionary sentencing guidelines, have led to Black people being highly over-represented in the US prison population. Black people make up 13 percent of the US population, but represent over 38 percent of the prison population. Many Covid-19 outbreaks have been documented in correctional institutions, including the five largest known clusters of Covid-19. In addition, the death rate from Covid-19 is higher in prison populations than it is in the general population.
We must implement short term measures and work towards long term solutions to address the current racial health disparities that Covid-19 has exacerbated and to ensure that we address long-standing inequity starting now. In the short term, community testing needs to be expanded, especially in communities of color, and turnaround time for results must be drastically reduced. Those who test positive for the coronavirus must be compensated to stay home and those who cannot isolate safely at home should be provided with free accommodation to do so. Health education on the coronavirus should be readily available in languages other than English. Data on Covid-19 disaggregated by race and ethnicity at the Federal Level must be provided more often to inform our response and the equitable allocation of resources.
In addition to these short-term measures, we must address the reality that the pandemic continues to highlight – that the US health system, and surrounding systemic structures, are deeply inequitable. In an article published in the New England Journal of Medicine, Dr. Michele K. Evans writes that “inequities in health, health care access, and quality of care are ingrained in the U.S. health care system. These inequities are not a sign of a broken system: in fact, in this sense, the system is operating just as it was built to operate.” We must reimagine and create a US health system that is well-funded, just, and equitable. A well-functioning health system must integrate with other sectors including education, housing, employment, and criminal justice if true health equity is to be achieved. We need to invest the necessary resources across sectors to improve health in the most marginalized communities.