Report 61: Histopathology Series Part 3 – Ute Krüger, MD, Breast Cancer Specialist, Reveals Increase in Cancers and Occurrences of “Turbo Cancers” Following Genetic Therapy “Vaccines”

This report is Part 3 in a series. It follows Part 1, “Report 56: Autopsies Reveal Medical Atrocities of Genetic Therapies Being Used Against a Respiratory Virus,” and Part 2, “Report 58: Part 2 – “Autopsies Reveal Medical Atrocities of Genetic Therapies Being Used Against a Respiratory Virus.”
A Lecture by Ute Krüger, MD, DMedSci
https://lakaruppropet.se/international-conference-pandemic-strategies/
Ute Krüger, MD, DMedSci, is a pathologist educated in Germany now living and working in Sweden. She wrote her doctoral thesis at the Humboldt University in Berlin on the analysis of 7,500 autopsy protocols. With over 25 years of experience in Clinical Pathology and a special interest in breast cancer, Ute has been researching breast cancer at Lund University for almost eight years. She was a member of the Board of the Swedish Association of Pathologists and was previously Medical Chief of the Department of Clinical Pathology in Växjö. She works as a Senior Physician in the Department of Clinical Pathology in Kalmar.
[Note: A rough draft was prepared using voice recognition that was then was edited for clarity with an effort to retain Dr. Krüger’s original meaning. The text was then added to the presentation graphics.]

Dr. Krüger, MD, is a pathologist who specializes in diseases of the breast. Her lecture concerned changes in breast cancer cases following introduction of Spike generating genetic drug therapy.
Ute Krüger, MD
“I’m very pleased to have the opportunity to speak as a member of the Physician’s Appeal, Läkaruppropet. Thank you all to my colleagues who organized this important conference and to all of you for coming.
You may be wondering about the title of my lecture. But more on that later.

At the beginning of the COVID-19 outbreak, I researched on the Internet and found that the mortality rate following infection with the coronavirus was around 2%. In comparison, sarcoidosis is an inflammatory disease, and the most important interstitial lung disease in Western Europe is described as having a mortality rate of just under 5%.
Have you ever heard anything in the media about sarcoidosis, which has a much higher mortality rate than COVID-19?
In addition, in medical school, I was given a different definition of the term “pandemic than we used today. In the period that followed, I observed the events very closely.”
I’ve been working in pathology for 25 years. For the last 19 years, I was mainly involved in the diagnosis of breast specimens. Almost eight years ago, I got the opportunity to work in breast cancer research at Lund University. Here I have reevaluated 1,500 breast cancer cases according to currently valid guidelines.
With this experience, I know approximately the distribution of average age, tumor size, and degree of malignancy that I can expect in the daily input material of breast cancer.

Already, in Autumn 2021, I had the impression that I was suddenly receiving more material
- From younger patients, often 30 to 50 years old.
- The tumors were growing more aggressively and faster.
- And that they were larger. More than four centimeters was not uncommon. I saw tumors up to 16 centimeters in size in the breast.
- I also had the impression that multifocal tumor growth and bilateral tumor growths were more frequent.
My efforts at the second pathology conference in Germany, in December 2021, to find colleagues to help me prove or disprove my hypothesis of Turbo Cancer after vaccination against COVID-19 met with little response.
I would like to go into detail. Since I love my microscope and pictures, I would like to show you some pictures from histology. Agent E stands for Hematoxylin Eosin (H&E) and is a routine stain in clinical histopathology.
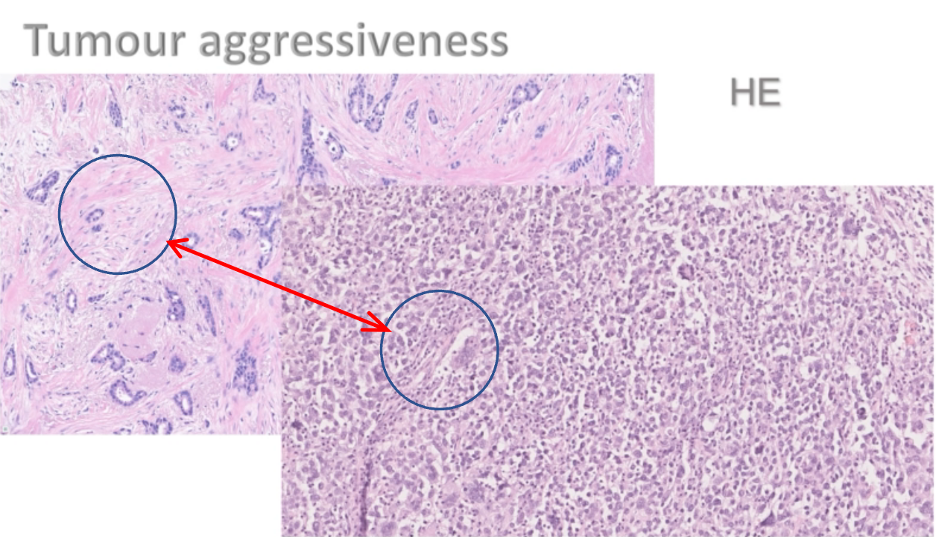
Tumor Aggressiveness
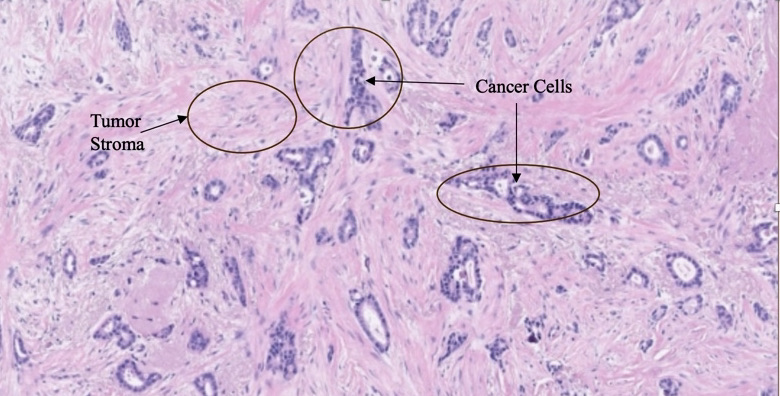
Here we see a breast carcinoma that is well differentiated. I think for most here it’s difficult to interpret histologic slides. So here are a few explanations.
- You see, small tumor glands, the dark ones here in a relative abundant stroma.
- The tumor cells are relatively small and about the same size.
In the next image you see a poorly differentiated, more aggressively growing tumor. (Below) You see a solid tumor mass with a very small amount of stroma.
The tumor cells are slightly larger.
There are also cells with huge cell nuclei.
But I chose this example because the proliferation activity. You will see the next picture is very important here to show how many tumor cells are dividing. There is an immunohistochemical stain, Ki67, which is a proliferation marker. About two-thirds of all breast cancers have a low proliferation. One-third of breast cancers are highly proliferative, meaning they grow faster and more aggressively.
I would like to show you the tumor shown in the previous picture stained with Ki67.
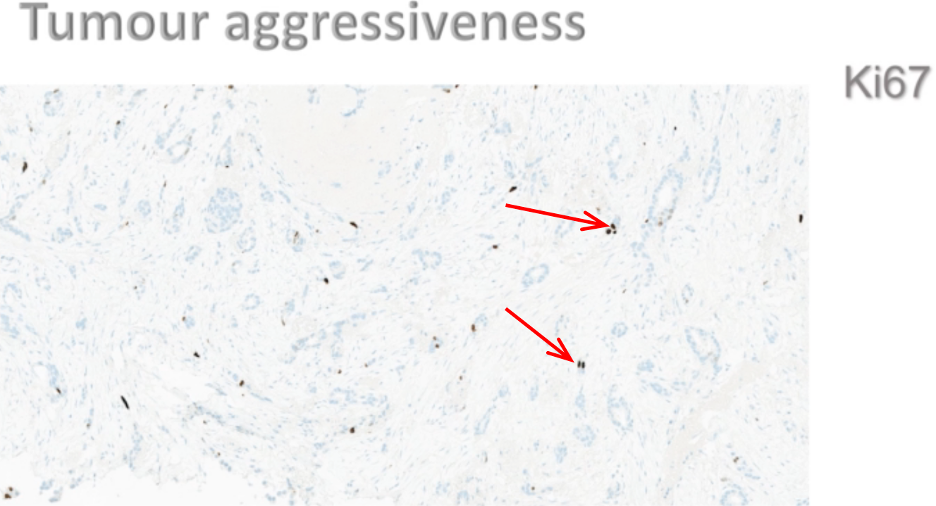
The first tumor (above) showed low proliferate proliferative activity. Less than 10% of the nuclei are stained brown, meaning they are in proliferation. You see the dots here.
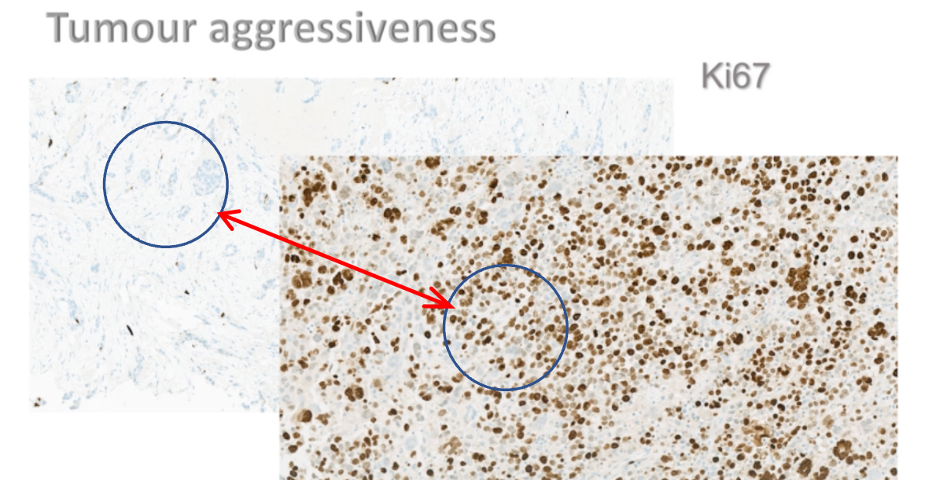
Here is the very fast-growing tumor with about 70% tumor cells staining brown. That means more than two-thirds of the tumor cells are in cell division. Such aggressively growing tumors seem to be more common in my routine material now.
Of course, the aggressiveness of is also reflected in the increased number of mitosis (arrows).
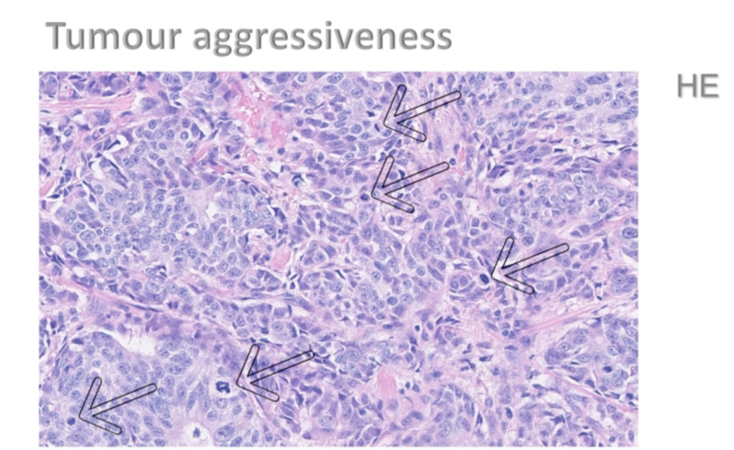
Here is another breast carcinoma. The mitoses are marked with arrows.
I see more and more multifocal tumors.
Multifocality
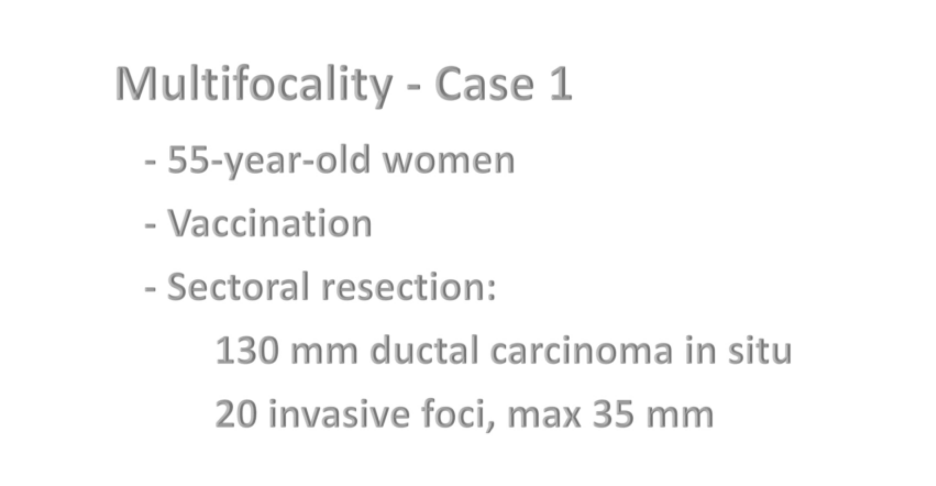
I found in her breast specimen a 130-millimeter ductal carcinoma in situ. That means a tumor growth in the mammary ducts. In the same area, I found 20 invasive foci of poorly differentiated ductal breast carcinoma. And the largest invasive focus was 35 millimeters.
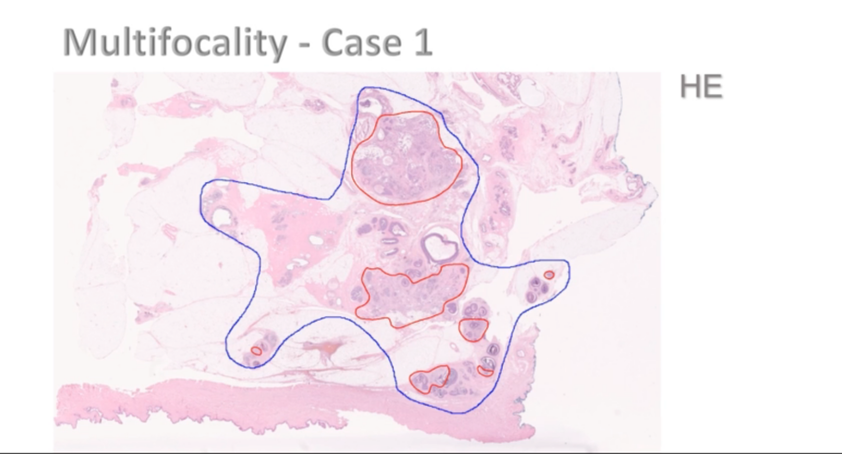
Here we see one of the slides. The area was ductal carcinoma in situ marked with blue. In this picture, you see seven different invasive foci marked with red. The tumor had short, pronounced growth in the lymphatic vessels, even far outside the actual invasive event in the breast, and four lymph nodes were already affected.
Recurrences
Another anomaly I think I see is recurrences. These are patients who have had breast cancer before and were more or less considered cured. It can be carcinoma from 20 years ago. Relatively soon after the vaccination against COVID-19, the tumor growth explodes, and there is a pronounced spread of the tumor in the body; and some of the patients die within a few months.
I will show you the case of an 80-year-old woman. Seven years ago, she had a sectoral resection, which means that part of her breast with the tumor was removed.
Three months after the vaccination against COVID-19, she was able to detect the tumor in her breast. It was a fast-growing tumor with a size of 55 millimeters in the surgical specimen.
At the same time, sever skin metastases were found in the breast skin of the same site. This is also very unusual for a patient with a recurrence in the breast and skin metastasis at the same time.
Here you can see the current specimen:
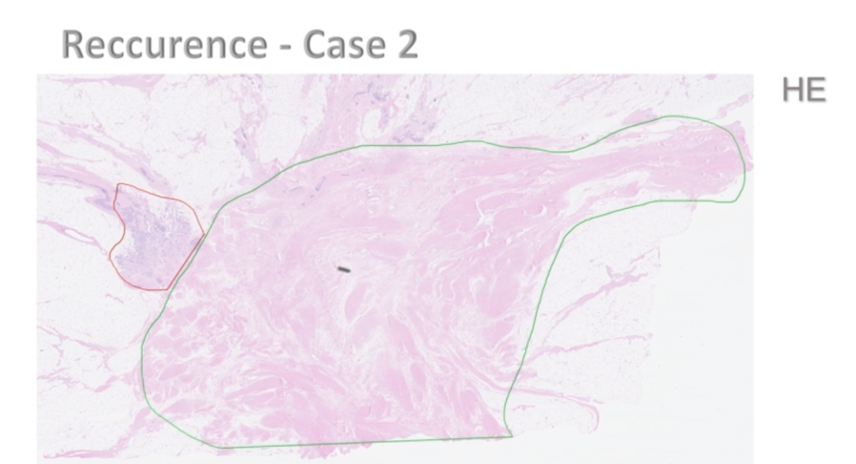
The area of the previous resection is marked in green and shows scar tissue. I hope you can see. This green is not the best color here. Right next into it, you can see the red area, and this is the recurrence. In this image, the direct proximity of the recurrence to the scar tissue was impressive.
Heterogeneity
The next aspect I would like to highlight is heterogeneity of the tumors. That means the tumor has different patterns.
I would like to show you an example of a 70-year-old woman. She had a lobular, that means relatively slow growing breast carcinoma, but she also had metastases for several years. She had been living with her metastases in the urinary bladder, the intestinal mucosa, bones, and liver for three years, and her body was in a certain balance.
Shortly after vaccination against COVID-19, the tumor growth in the liver exploded, and the patient died within a month. The doctor who sent me the liver sample wrote on the referral that it was unusual that the metastasis and the liver grew extremely fast, but the tumors in the other metastatic sites in her body did not grow at the same rate.
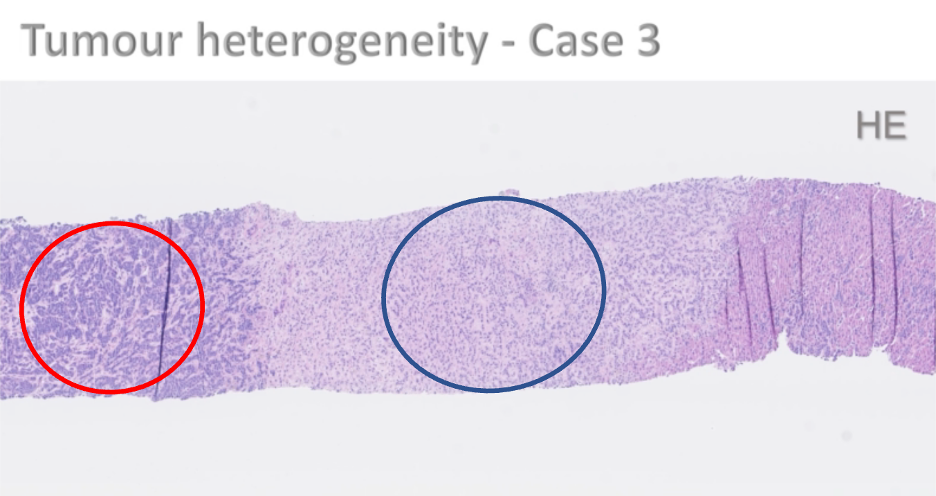
In the liver biopsy, in the microscope image on the right (referring to projection screen) here, you can see predominantly tumor-free liver tissue in the middle. (Blue circle) You see the known metastasis of lobular breast carcinoma with relatively small cell nuclei and clearly visible stroma. And on the left side you see the aggressively growing, newly added tumor with more compact tumor growth. (Red circle)
Coincident Tumors
Another anomaly is coincident tumors. Last year I had three patient cases within three weeks with three concurrent carcinomas in different organs (inaudible). This a few months after vaccination against COVID-19.
For example, I received a sample of breast carcinoma from a woman who had been diagnosed with primary lung carcinoma and primary pancreatic carcinoma at the same time. This is very unusual and remarkable. The tumor conferences are becoming more and more complicated. At my last breast cancer conference, I had 35 persons, some which were guests.
I have always worked in such smaller hospitals like this and never had so many patients at a tumor conference in the last 19 years before. A Swedish colleague, someone who works mainly as a neuropathologist, confirmed to me that tumor conferences are becoming more and more complicated. It’s not unusual for patients to have several malignancies in different organs at the same time.
Benign Tumors
Now I would like to talk about benign tumors in the breast. Another anomaly I think I see is appearance of larger fibroepithelial tumors.
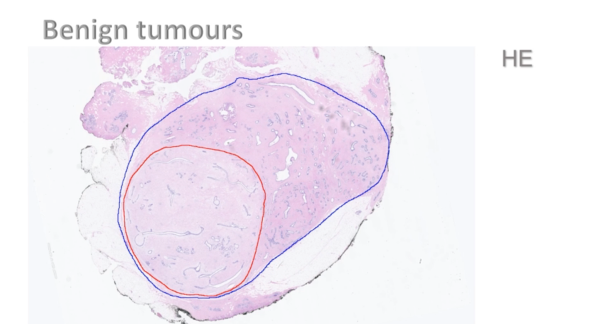
Here we see an example of fibroadenoma marked in blue. More than two-thirds of the fibroadenoma shows a little proliferative stroma in this part of the fibroadenoma. It has not grown in the last few months.
The area highlighted in red is the proliferative area in the tumor. The stroma was loosened (sic) with proliferative activity.
I see such changes with proliferative areas in already existing fibroadenomas more frequently now. I also see fibroadenomas that are proliferative active through.
Inflammation
Sometimes I get the clinical information that the patient comes to the doctor because of pain and the palpation finding, and it’s possible that the cause of the pain is inflammation.
It’s not uncommon for me to see inflammatory cells both in the tumor and in the surrounding tissue.
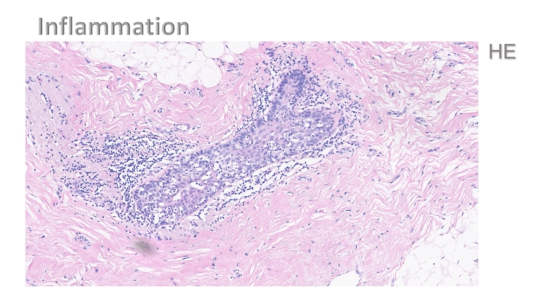
Here you see a milk duct with a periductal here in the stroma and intraepithelial, lymphocytic infiltrates. The lymphocytes are the small dark dots you see.
It’s not uncommon for me to see vasculitis like changes in the mammary parenchyma. That means inflammation in the small vessels in the breast.
Now back to the tumors.
After my interview with Miriam Reichel one year ago about turbo cancer and vaccination against COVID-19, there are more than 1,300 comments. Among them are numerous reports of turbo cancer cases from personal experience, friends, or relatives.
I have picked out one comment, and I would like you to read it for yourself. I hope you can see this in the back. Yes.
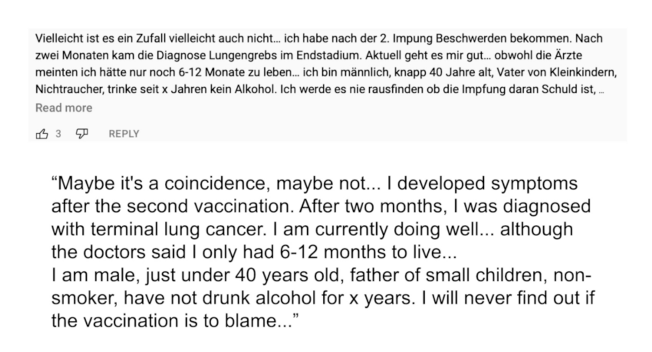
Again, you can see that the patient’s age and lifestyle habits do not match such an aggressive lung cancer, and it’s a very unusual course.
After my lecture in Oslo to Norwegian doctors and nurses in June last year, I also received a lot of feedback. On the one hand, there are case descriptions from affected patients or their relative. And on the other hand, colleagues who confirm my theory that rapid tumor growth seem to be related to the vaccination against COVID-19.
Unfortunately, I’m also contacted by patients who urgently need help because of severe side effects or turbo cancer cases after these vaccinations. They are simply not taken seriously by the doctors treating them, because, in the eyes of most of doctors, there are no side effects of the vaccinations against COVID-19.
Unfortunately, I cannot help these patients.
Statistics
What about the statistics? I try to evaluate the number of breast carcinoma cases in our institute over the last few years. At first, I was disappointed because I could not find any trend in the number of cases, the average age of the patients and the average tumor size. On second thought, however, I realized that the evaluation of data cannot be that simple.
Fortunately, the suspected link between COVID-19 vaccination and turbo cancer does not apply to everyone. In the cases of so-called turbo cancer, the patients often receive neoadjuvant chemotherapy – that means chemotherapy before surgery because of the large tumor size. In our statistical system at the institute, only the tumor size of the surgical specimen and not the original tumor size as recorded.
In all breast cancer cases, the so-called HER-2 (https://www.mayoclinic.org/breast-cancer/expert-answers/faq-20058066) status and the hormone receptor status are examined by pathologists. HER-2 is a protein to help tumor cells grow faster, so HER-2 positive breast cancer grows quickly. There are also so-called triple-negative tumors, which means that hormone receptors and HER-2 status are negative.
Triple-negative tumors also grow quickly. These HER-2 positive and also triple-negative tumors are often treated with neoadjuvant chemotherapy. It’s not uncommon to see pathologic complete response. That means the tumor has disappeared, and the tumor site on the surgical specimen is zero millimeters.
Of course, this affects the statistics.
Actually, we should investigate all cases with tumor growth after vaccination against COVID-19. Multifocal and bilateral tumor growth would need to be recorded. For reliable statistics we would need more case numbers from multiple institutes – preferably cross-national collecting and analyzing data to prove or disprove my hypothesis of post-vaccination turbo cancer.
Now, you may wonder why I choose such a strange title for my lecture. I found the painting by the Swedish artist (unrecognizable Swedish name). That fits very well. But after 18 years in Sweden, I can tell you this is not the usual way of fishing here in Sweden.

In September 2022, the press in Sweden became aware of my performance in Oslo. Regional Radio interviewed the head of the Kalma Hospital, Johan Rosenquist, and Mr. Rosenquist commanded that it would take many more cases to investigate my statement and that there would be no consequences for me after this talk as I was allowed to speak as a private person.
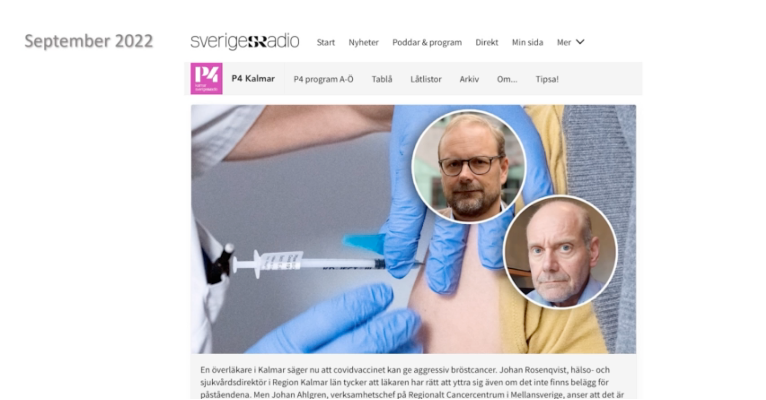
But this man here, Johan Ahlgren, the head of the mid-Sweden regional cancer center, a lecturer in oncology, calls my approach sabotaging the region’s efforts to get everyone vaccinated.
I think if my theory had been wrong, no one would have cared what I said.
Now pathologists are usually associated with autopsies, but these make up a very small part of a pathologist’s work these days. I have only done single autopsies recently, but there are three deaths that I strongly suspect are related to the vaccination against COVID.
I published one of these cases four months ago.
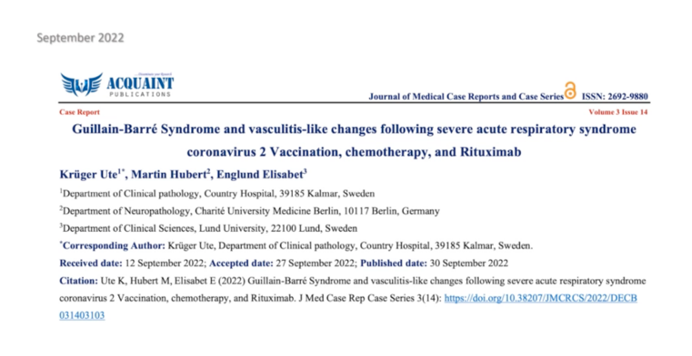
Unfortunately, there’s not enough time to go into detail. Here’s the title if you want to go know more about it. The other cases, short, similar findings to those that Professor Burkhardt, I will show you in a moment.
However, I see four major problems with autopsies.
- No postmortem examination is carried out. It’s the first one, the second one.
- Incorrect information given by the clinician when asked whether the deceased have been vaccinated. I have seen more than one case in our hospital where the clinician noted on the referral for autopsy that the deceased had not been vaccinated. However, I found in the patient’s journal that the patient had indeed been vaccinated against COVID-19.
- The third is many of the pathologist colleagues do not take samples for histological examination – that means no microscopic examination is performed. Without microscopy, you cannot see, for example, myocarditis or vasculitis.
- And the fourth is the lack of knowledge in the assessment of microscopic findings.
‘You only see what you know.’
Goethe
Goethe lived 200 years ago. Goethe was a German poet and naturalist. He’s considered one of the most important creators of German language poetry. And, slightly modified by me,
‘You only see what you know.
And
What you want to see.’
The changes I have described, which seem to be related to the COVID-19 vaccination are only a small part of what happens in the body.
I can say that I haven’t given up. I studied medicine because I want to help people.
But now it feels like I’m watching people being killed and I cannot do anything. As a pathologist, I diagnose tumors that maybe have been caused by another colleague with a shot.
This is completely pointless and absurd.
Over the last year, I have been exploring many alternative healing methods, our nutrition, the power of our nature, and our wild herbs.
I want to bring you closer to the beauty of our nature. Here, for dinner last summer, I collected leaves and flowers from 35 different bushes, perennials, and wild herbs in my garden to eat, and I am still alive.
Among other things, these give me strength and confidence for the future.
Thank you very much for your attention.”
Ute Krüger, MD, DMedSci
Summary:
Following widespread distribution and injection of Spike-producing therapeutics, Dr. Krüger noticed a number of changes on which she was asked to consult:
- Younger patients are being seen, often 30- to 50-year- old.
- Tumors are growing more aggressively and faster.
- Tumors are larger.
- Tumors exhibit heterogeneity.
- Multifocal tumor growth and bilateral tumor growths are more frequent.
- Co-temporal onset of more than one type of cancer.
- Benign tumors have accelerated growth possibly signifying malignant transformation.
- The physiologic process of inflammation was noted as a possible source of breast pain.



What evidence is there that the cases spoken about in this article are anything more than relatively isolated examples? I am in the medical field, Radiology, and have heard nothing from oncologists or anyone else about any major change in the typical courses of breast cancer patients, or patients with other types of malignancies. Not have I seen any dramatic difference in the PET/CT’s, bone scans, CT scans, and other studies that are used to follow these patients and affect treatment decisions.
Well, they most probably didn’t open their eyes.
I am a medical researcher too.
Thank you doctor for your work, and for being sensible and brave .
Congrats!