Opinion: “Why Not Vitamin D For All?”
Watch Dr Naomi Wolf’s Interview With Dr Vatsal G. Thakkar HERE
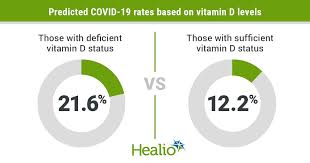
Studies about the effects of vitamin D on Covid-19 started trickling in a year ago. What started out as a highly plausible theory was quickly bolstered by dozens of observational studies showing that the lower one’s blood level of vitamin D, the higher the likelihood of SARS-CoV-2 infection as well as the severity of Covid-19. With this steady stream of science, I honestly thought health care leaders and public officials would notice and take action. They didn’t.
Then summer was upon us and Covid-19 hospitalizations and deaths started to fall, despite a surge of cases across the United States. It’s human nature to believe this was due to our actions, our mastery over this virus. Talking heads on TV stated this was possibly due to more young people being infected, or perhaps that we finally knew how to better treat patients with Covid-19. But when I dug into that data, I knew it not to be true (this was even admitted to by Dr. Chris Murray, director of the Institute for Health Metrics & Evaluation). However many of us who have studied vitamin D as well as the history of respiratory infections knew that deaths would spike again in the fall and winter, and unfortunately they have. So how does vitamin D relate?
We cannot get enough vitamin D from food—most of it needs to be made from direct sunlight when ultraviolet-B rays hit a specific cholesterol molecule in our skin. Since nearly each one of our cells contains vitamin D receptors, its impact goes well beyond helping strengthen our bones, which has been known for a hundred years. Our levels rise in the summer and because vitamin D is fat-soluble, slowly fall through winter, bottoming out by March. Fifteen minutes a day of direct mid-day sun between April and October is all most people need in the northern hemisphere, but only if they are young, thin and white. Obesity causes vitamin D to be sequestered in fat cells, leaving less available for necessary functions. Aging reduces the 7-dehydrocholesterol molecule in the skin dropping natural vitamin D synthesis by fifty percent. And darker skin can require triple the amount of sunlight for adequate vitamin D production because melanin blocks UV-B rays, which is why more than half of the U.S. Black population is deficient. These vitamin D deficient populations are the same ones who continue to show the highest mortality rates with coronavirus infections.
Millions of Americans have previously been told that they are low in vitamin D—but how is this suddenly more dangerous this year than last? The SARS-CoV-2 virus can overcome its host with a fatal trifecta—getting past the body’s defenses to infect respiratory cells, triggering a massive immune system overreaction (a cytokine storm), then culminating in respiratory failure known as ARDS (acute respiratory distress syndrome). Studies show that vitamin D, a potent immunomodulator, provides robust protection at each one of these steps.
How can we separate out the effects of vitamin D from other factors? Studying the effect of skin tone at different latitudes can be illustrative. Take the fact that Africans near the equator seem to be experiencing much milder cases of Covid-19, suggesting that stronger UV-B exposure, and therefore higher vitamin D levels, might be protective. Conversely, we also have data on individuals of African descent at higher latitudes, for example in Scandinavia, where healthcare is universal and poverty is low, but sunlight is weaker. Somali immigrants in Sweden were found to have mortality rates from Covid-19 four times higher than other Swedes after factoring for social determinants of health. But this disparity only appeared for coronavirus infections—the mortality rate from other diseases among Somali immigrants there showed little to no ethnic disparity.
The best evidence for causality has come in just the last few months—several randomized controlled trials have shown that aggressive vitamin D supplementation (on the order of 50,000 IU per day for 7-10 days) resulted in fewer complications, fewer ICU admissions and fewer deaths. This should be groundbreaking news—a way to stem the death toll immediately. But again, we have heard nothing from those who set health policy.
The 1918 influenza pandemic killed almost 700,000 Americans, a number we are fast approaching with this pandemic. Researchers have shown that more people died in the northern United States back in 1918—New London, Connecticut had a fatality rate almost four times higher than San Antonio, Texas. An analysis was performed across 88 countries showing a similar latitude distribution in Covid-19 deaths–countries further from the equator fared worse. More sun exposure, with its higher vitamin D production, might have played a protective role a century ago and may well play one now.
What needs to be done? Our leaders need to “follow the science” as they so often claim to do. They need to listen to the advice of former Surgeon General Richard Carmona, MD, MPH and aggressively treat vitamin D deficiencies in Covid-19 patients. They need to listen to the recommendations in the Vitamin D For All open letter, signed by over 200 international doctors and scientists including epidemiologists, critical care specialists and vitamin D researchers from places like Harvard, Princeton, and Yale. They need to raise public awareness about vitamin D supplementation and emphasize it at least as much as they do mask-wearing as a preventative measure.
Dr. Anthony Fauci, our most beloved public health official, admitted that vitamin D can lessen susceptibility to coronavirus infection and reportedly takes 6000 IU of it daily, almost eight times his recommended daily allowance. Why can’t he advise all Americans to do the same? Please join our campaign to tell our leaders to recommend vitamin D for all.




