“Covid-19 Vaccine Protocols Reveal That Trials Are Designed To Succeed”
Moderna, Pfizer, AstraZeneca, and Johnson & Johnson are leading candidates for the completion of a Covid-19 vaccine likely to be released in the coming months. These companies have published their vaccine trial protocols. This unusually transparent action during a major drug trial deserves praise, close inspection of the protocols raises surprising concerns. These trials seem designed to prove their vaccines work, even if the measured effects are minimal.
What would a normal vaccine trial look like?
Prevention of infection must be a critical endpoint. Any vaccine trial should include regular antigen testing every three days to test contagiousness to pick up early signs of infection and PCR testing once a week to confirm infection by SARS-CoV-2 test the ability of the vaccines to stave off infection. Prevention of infection is not a criterion for success for any of these vaccines. In fact, their endpoints all require confirmed infections and all those they will include in the analysis for success, the only difference being the severity of symptoms between the vaccinated and unvaccinated. Measuring differences amongst only those infected by SARS-CoV-2 underscores the implicit conclusion that the vaccines are not expected to prevent infection, only modify symptoms of those infected.
We all expect an effective vaccine to prevent serious illness if infected. Three of the vaccine protocols—Moderna, Pfizer, and AstraZeneca—do not require that their vaccine prevent serious disease only that they prevent moderate symptoms which may be as mild as cough, or headache.
The greatest fear people have is dying from this disease. A vaccine must significantly or entirely reduce deaths from Covid-19. Over two hundred thousand people have died in the United States and nearly a million worldwide. None list mortality as a critical endpoint.
We recognize that the influenza vaccine does not prevent infection with that virus, but does have a measurable impact on hospitalization and death. The moderate protections from the influenza virus can potentially be replicated and improved on with Covid-19, but only with extensive trials that ensure the efficacy of a future vaccine.
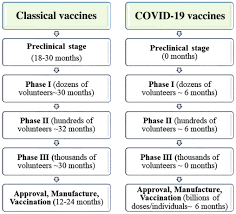
Vaccine efficacy is typically proved by large clinical trials over several years. The pharmaceutical companies intend to do trials ranging from thirty thousand to sixty thousand participants. This scale of study would be sufficient for testing vaccine efficacy. The first surprise found upon a closer reading of the protocols reveals that each study intends to complete interim and primary analyses that at most include 164 participants.
These companies likely intend to apply for an emergency use authorization (EUA) from the Food and Drug Administration (FDA) with just their limited preliminary results.
Interim analysis success requires a seventy percent efficacy. The vaccine or placebo will be given to thousands of people in each trial. For Moderna, the initial interim analysis will be based on the results of infection of only 53 people. The judgment reached in interim analysis is dependent upon the difference in the number of people with symptoms, which may be mild, in the vaccinated group versus the unvaccinated group.
Moderna’s success margin is for 13 or less of those 53 to develop symptoms compared to 40 or more in their control group. For Johnson & Johnson, their interim analysis includes 77 vaccine recipients, with a success margin of 18 or less developing symptoms compared to 59 in the control group. For AstraZeneca, their interim analysis includes 50 vaccine recipients, with a success margin of 12 or less developing symptoms compared to 19 in the 25 person control group. Pfizer is even smaller in its success requirements. Their initial group includes 32 vaccine recipients, with a success margin of 7 or less developing symptoms compared to 25 in the control group.
The primary analyses are a bit more expanded, but need to be less efficacious for success: about sixty percent. AstraZeneca, Moderna, Johnson & Johnson, and Pfizer have primary analyses that distribute the vaccine to only 100, 151, 154, and 164 participants respectively. These companies state that they do not “intend” to stop trials after the primary analyses, but there is every chance that they intend to pursue an EUA and focus on manufacturing the vaccine rather than further thorough testing.
The second surprise from these protocols is how mild the requirements for contracted Covid-19 symptoms are. A careful reading reveals that the minimum qualification for a case of Covid-19 is a positive PCR test and one or two mild symptoms. These include headache, fever, cough, or mild nausea. This is far from adequate. These vaccine trials are testing to prevent common cold symptoms.
These trials certainly do not give assurance that the vaccine will protect from the serious consequences of Covid-19. Johnson & Johnson is the only trial that requires the inclusion of severe Covid-19 cases, at least 5 for the 75 participant interim analysis.
One of the more immediate questions a trial needs to answer is whether a vaccine prevents infection. If someone takes this vaccine, are they far less likely to become infected with the virus? These trials all clearly focus on eliminating symptoms of Covid-19, and not infections themselves. Asymptomatic infection is listed as a secondary objective in these trials when they should be of critical importance.
It appears that all the pharmaceutical companies assume that the vaccine will never prevent infection. Their criteria for approval is the difference in symptoms between an infected control group and an infected vaccine group. They do not measure the difference between infection and noninfection as a primary motivation.
A greater concern for the millions of older people and those with preexisting conditions is whether these trials test the vaccine’s ability to prevent severe illness and death. Again we find that severe illness and death are only secondary objectives in these trials. None list the prevention of death and hospitalization as a critically important barrier.
If total infections, hospitalizations, and death are going to be ignored in the preliminary trials of the vaccines, then there must be phase four testing to monitor their safety and efficacy. This would be long term massive scale monitoring of the vaccine. There must be an indication that the authorized vaccines are reducing infection, hospitalization, and death, or else they will not be able to stop this pandemic.
These protocols do not emphasize the most important ramifications of Covid-19 that people are most interested in preventing: overall infection, hospitalization, and death. It boggles the mind and defies common sense that the National Institute of Health, the Center for Disease Control, the National Institute of Allergy and Infectious Disease, and the rest would consider the approval of a vaccine that would be distributed to hundreds of millions on such slender threads of success.
It appears that these trials are intended to pass the lowest possible barrier of success. As this is being written, the FDA is poised to announce tougher standards for a Covid-19 vaccine in the near future. It is my hope that these new standards for an EUA will at a minimum include requirements for protections from infection itself, protections from severe virus-related disease leading to hospitalization, and a significant improvement in Covid-19 related mortality.
It is clear from these studies that the vaccines currently under trial will not be the silver bullet needed to end the pandemic. We must do all we can public health measures to control Covid-19 as China and other Asian countries have successfully done.
Reprinted with permision. This article originally appeared on Forbes.com