Report 64: Histopathology Series Part 4a – Re-Humanizing Data Using “Intramyocardial Inflammation after COVID-19 Vaccination: An Endomyocardial Biopsy-Proven Case Series.”
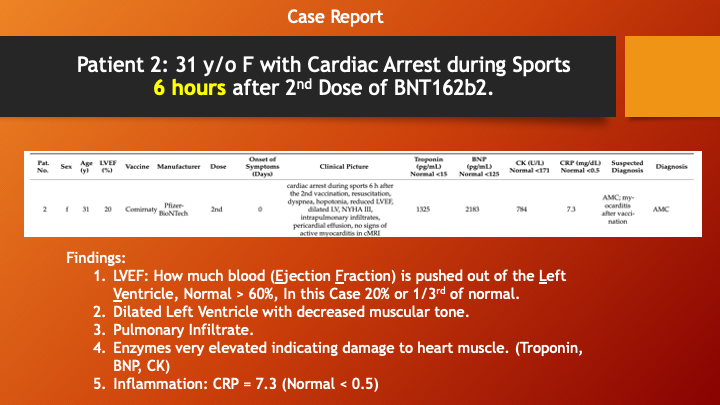
A 31-year-old woman participating in athletics suffered a cardiac arrest six hours after her second dose of BNT162b2, Pfizer’s COVID-19 mRNA gene therapy “vaccine.”
Following successful resuscitation, she was found to have shortness of breath and a weakly beating heart. Her cardiac output, as measured by her left ventricle ejection fraction (LVEF), was about one-third normal blood flow out of her heart.
Blood studies indicated severe heart injury. A biopsy from inside her heart was thoroughly analyzed using conventional and special stains, and it showed a pattern different from common causes of cardiac arrest. It pointed to autoimmunity caused by the LNP/mRNA injection.
The following article demonstrates how to extract data from Tables and Figures to understand the medical “work-up” and how causation can be explored with special diagnostic techniques.
These techniques should be applied to many of the “Died Suddenly” cases showing up around the world in order to understand the mechanism of injury and, in the cases of novel gene therapy products, to develop specific treatments.
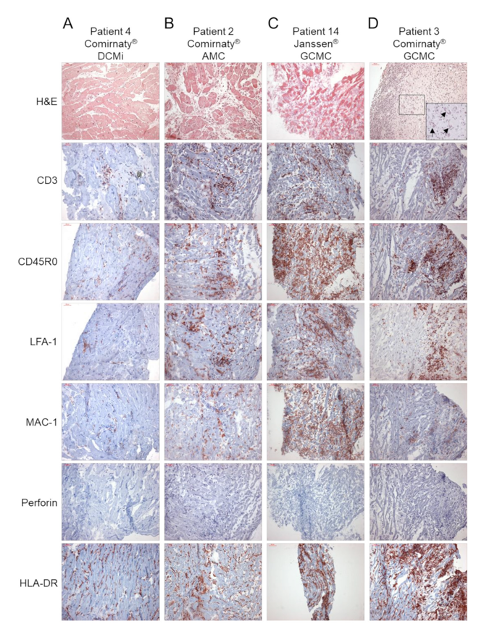
They collected 15 cases of myocarditis following injection of Lipid Nanoparticle LNP/Messenger RNA (mRNA) or Adenovirus-vectored DNA coded to produce Spike proteins. The 15 cases were worked up with cardiac diagnostic studies (Table 1) and cardiac biopsy from inside the heart (endomyocardial biopsy) (Table 2 and Figures 1 and 2).
The specimens were then carefully analyzed histologically using immunohistochemical techniques to determine cellular events in damaged heart muscle. Virologic analysis was done. The diagnostic data is presented two tables and three figures.
The second and third sentences identify what the authors believe to be important about their research, namely biopsy-obtained histology in severe cases of myocarditis following injection of Spike generating COVID-19 therapeutics.
The natural inclination is to attempt to read this article from first to last sentence, but this approach may present a challenge due to densely packed and largely unfamiliar nomenclature and complex medical concepts.
This article will show a way to penetrate this dense, data rich material using an incremental mining approach without a cover-to-cover read. Open the Baumeier, et al. paper and follow along.
Let us begin with Table 1 on page 3:
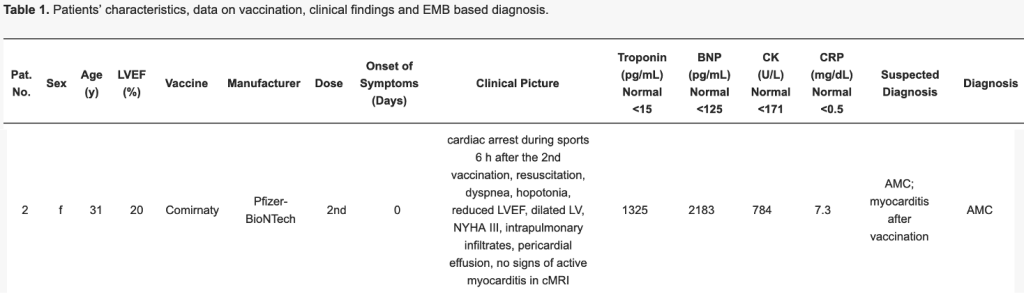
Patient 2 is selected because she is a woman (72% of adverse events), who is young, 31 , was engaged in sports activity when her heart stopped 6 hours after receiving dose 2 of BNT162b2, Column 9.
She had emergency treatment (resuscitation) and was identified as having shortness of breath and a weakly beating heart (hypotonia).
LVEF stands for left ventricle ejection fraction, which is the amount, as a percentage, of blood the left, lower chamber of the heart forces out with each contraction. Normal LVEF is above 52% (https://www.onlinejase.com/article/S0894-7317(21)00761-6/fulltext and https://www.healthline.com/health/ejection-fraction#ejection-fraction-results), although there is some variability in reported normal values. (Low normal is in the 52-60% range but as an athlete hers was probably >60%.)
Looking in column 4, we see Patient 2 had a left ventricular ejection fraction of 20%, a reduction of almost two-thirds. This means that following her resuscitation, her cardiac output was severely reduced, she had fluid in her lungs, and fluid around her heart between the heart muscle and the fibrous membrane around the heart muscle (pericardium).
Interestingly, these profound changes were not picked up on cardiac magnetic resonance imaging (false negative cMRI). We do not know if they used a contrast agent called Gadolinium which can enhance the imaging.
So, we have looked at nine columns and have learned quite a lot about this woman’s unfortunate medical situation. She almost died, and her heart is seriously compromised. And the cardiac arrest happened just six hours her second after BNT162b2 injection. We do not know whether there was a silent myocarditis from first injection. The fact that she was participating in athletics at the time of her cardiac arrest suggests that this was a sudden, catastrophic process with close temporal proximity to receiving a dose of BNT162b2 as has been implicated in other similar cases (DOI: 10.1007/s00392-022-02129-5 ).
Columns 10 through 14 contain results of blood studies indicating heart damage sufficient to release products into the bloodstream that can be measured, troponin, B-type natriuretic peptide (BNP), and creatine kinase (CK). These are discussed more fully below. The suspected diagnosis is given as acute myocarditis following BNT162b2, but the diagnosis omits the association between BNT162b2 and the myocarditis. Some hedging is probably allowable for now.
A biopsy was taken from inside the heart and carefully analyzed histologically. The results of the biopsy with special staining are presented in column B for Patient 2. The rest of Figure 2 is about other patients which we will ignore for now. The legend to Figure 1 is dense and perhaps a bit off putting because of unfamiliar nomenclature. For now, just have a look and observe that there are seven different stains applied to the biopsy specimen.
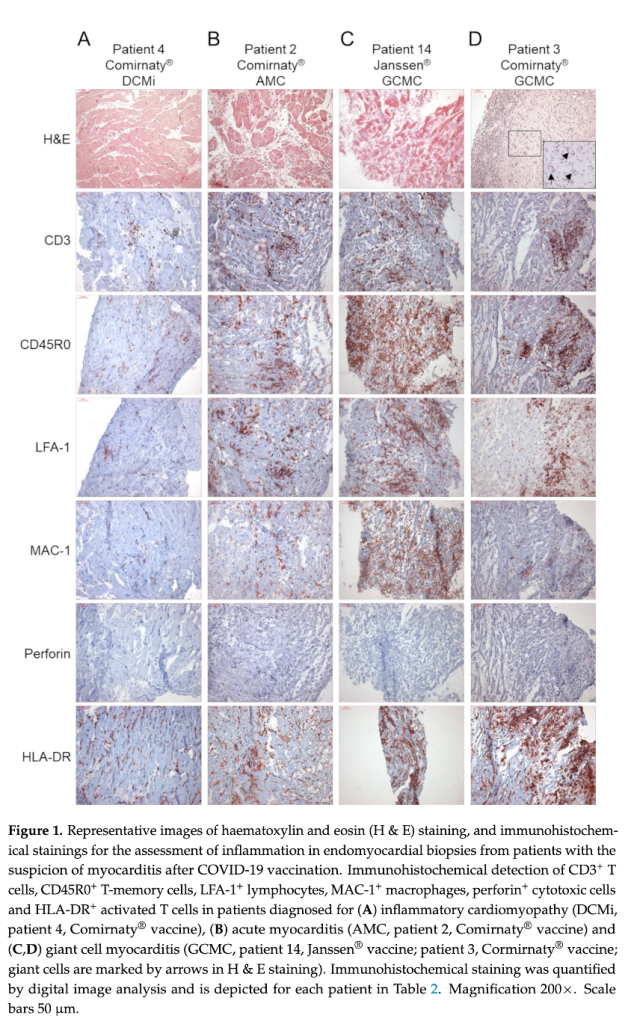
The first stain, Hematoxylin and Eosin (H&E), is very common, but the remaining ones are special stains for this diagnosis, myocarditis. This densely packed figure will be broken down below so be curious but keep going.
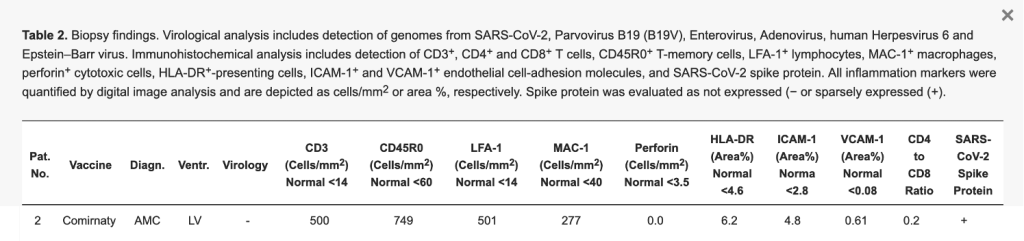
Table 2 is also packed with information including the patient identifier, the vaccine, the diagnosis of “AMC,” which stands for Acute Myocarditis. The site of the biopsy is “LV” for left ventricle. The next column reports no evidence of virus in the patient on molecular testing.
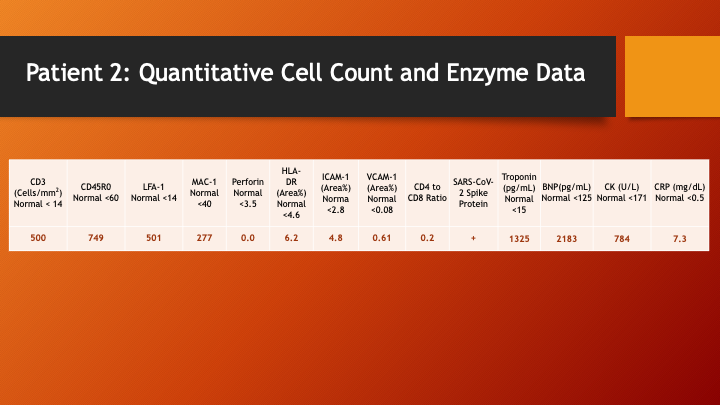
Now, we get to a fascinating and unique aspect of this study, quantitative measurements of the type of cells and other substances that accumulated in this woman’s heart muscle and that should not be present in the numbers measured. The complexity of this study just took a giant step up. What are all those measurements? Time to dig.
But first, let’s recap (this is how the case might be presented in a lecture):
Call this the “Clinical Picture” and caption it “Major Pump Failure” temporally related to an injection.
Next slide, please:
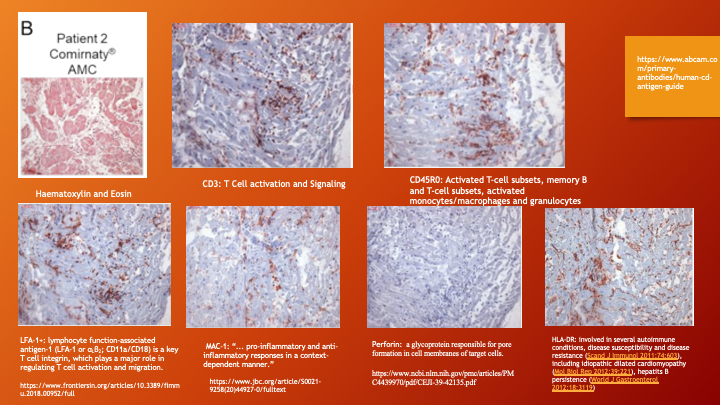
Here each treatment of the biopsy material is given its own box with labelling. This is way too busy for a lecture unless each of the seven boxes is discussed separately and given adequate time. In written format, the reader can take the time needed for a “first cut” read. So have a look and understand that there is a lot going on that should not be going on.
Take the top left box, common stain H&E. What does it show? Below is a cross-sectional view of cardiac muscle with red bundles (Eosin staining) with occasional blue (Hematoxylin or Basophilic stain) that identifies muscle cell nuclei (myocytes) that are located inside the fibrous wrapping (epimysium) of the muscle bundle. There is some white material, more fibrous material, containing the muscle bundle and its cell separating the muscle and muscle cell bundles but with no cells in between the bundles. Look past the depth of the red color (technique) to the density of the muscle bundles and observe that there are fewer healthy-looking muscle bundles on the left compared with normal on the right.
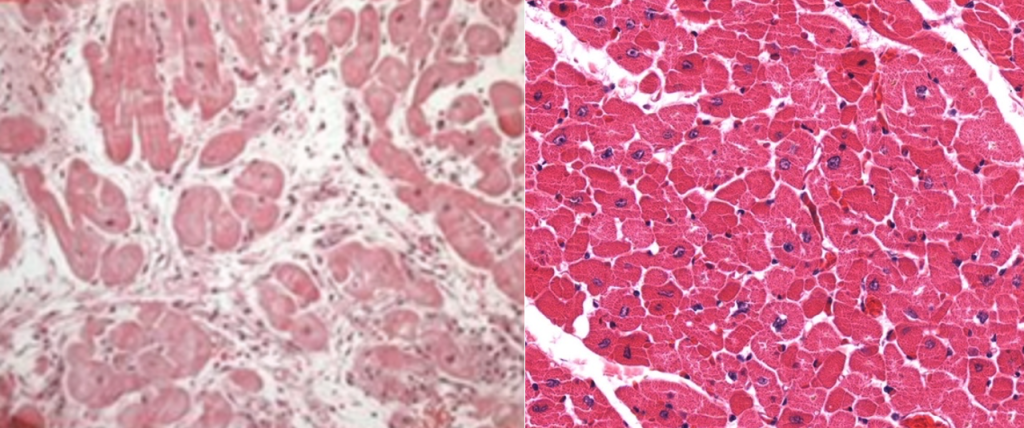
Patient 2 has more “stuff” between the bundles and, therefore, fewer bundles per field (check the magnification, not provided here but they seem roughly comparable). The “stuff” is cellular and probably contains excess tissue fluid. There are numerous cells outside of the muscle bundles in Patient 2. This is not normal.
Now, back to those cells that are not in the normal heart muscle. Here is where this study stands out. Many histology reports end here. But our German colleagues have gone further. What are those cells doing there, and how does this inform us about the disease process?
Now we can dive in and try to answer that question. Are these because of the cardiac arrest and are, therefore, acute inflammatory cells or substances related to the trauma of the cardiac arrest or were they there before the arrest occurred? This gets to causation. Can this be answered unequivocally?
Time to take it to the next level. Here is an explanation of the columns in greater detail. [Note: The text is quoted from the reference cited.]
- CD3: T-cell development and signal transduction. https://www.abcam.com/primary-antibodies/human-cd-antigen-guide
- CD45RO: Activated T-cell subsets, memory B- and T-cell subsets, activated monocytes/macrophages and granulocytes. https://www.abcam.com/primary-antibodies/human-cd-antigen-guide
- LFA-1+: lymphocyte function-associated antigen-1 (LFA-1 or αLβ2; CD11a/CD18) is a key T-cell integrin, which plays a major role in regulating T-cell activation and migration. https://www.frontiersin.org/articles/10.3389/fimmu.2018.00952/full
- MAC-1: … pro-inflammatory and anti-inflammatory responses in a context-dependent manner. https://www.jbc.org/article/S0021-9258(20)44927-0/fulltext
- Perforin: a glycoprotein responsible for pore formation in cell membranes of target cells. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4439970/pdf/CEJI-39-42135.pdf
- HLA-DR: involved in several autoimmune conditions, disease susceptibility, and disease resistance (Scand J Immunol 2011;74:603), including idiopathic-dilated cardiomyopathy (Mol Biol Rep 2012;39:221) and hepatitis B persistence (World J Gastroenterol 2012;18:3119)
- ICAM-1 (Area%) Normal <2.8: ICAM-1 is a cell surface glycoprotein and an adhesion receptor that is best known for regulating leukocyte recruitment from circulation to sites of inflammation. However, in addition to vascular endothelial cells, ICAM-1 expression is also robustly induced on epithelial and immune cells in response to inflammatory stimulation. Importantly, ICAM-1 serves as a biosensor to transduce outside-in-signaling via association of its cytoplasmic domain with the actin cytoskeleton following ligand engagement of the extracellular domain. Thus, ICAM-1 has emerged as a master regulator of many essential cellular functions both at the onset and at the resolution of pathologic conditions. https://academic.oup.com/jleukbio/article/108/3/787/6884318?login=false
- VCAM-1 (Area%) Normal <0.08: the vascular cellular adhesion molecule-1 (VCAM-1) is a protein that canonically participates in the adhesion and transmigration of leukocytes to the interstitium during inflammation. VCAM-1 expression, together with soluble VCAM-1 (sVCAM-1) induced by the shedding of VCAM-1 by metalloproteinases, have been proposed as biomarkers in immunological diseases, cancer, autoimmune myocarditis, and as predictors of mortality and morbidity in patients with chronic heart failure (HF), endothelial injury in patients with coronary artery disease, and arrhythmias. https://www.sciencedirect.com/science/article/pii/S0925443921001034?via%3Dihub
- CD4 to CD8 Ratio: Ratios between 1.5 and 2.5 are generally considered normal; however, a wide heterogeneity exists because sex, age, ethnicity, genetics, exposures, and infections may all impact the ratio. In the HIV negative population, a low CD4/CD8 immune risk phenotype reflects immune senescence, is associated with wide-ranging pathology and may also predict morbidity and mortality. Irreversible disruption of self-immunologic tolerance to endogenous antigens is a hallmark of autoimmune disease. In this setting of immune dysfunction, an abnormal CD4/CD8 ratio can emerge. Furthermore, while an abnormal ratio is not uniformly present in all autoimmune diseases, a decreased CD4/CD8 ratio is consistently seen in systemic lupus erythematosus. A low CD4/CD8 ratio reflects β-cell destruction and may predict diabetes diagnoses in first-degree relatives of type 1 diabetic probands. In a population study of solid neoplasms, an inverted CD4/CD8 ratio is associated with metastatic disease as compared with cancer patients without metastasis. Moreover, following acute myocardial infarction and cardiopulmonary resuscitation, a fixed low CD4/CD8 ratio is a poor prognostic sign. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5667733/pdf/ppat.1006624.pd
- Troponin (pg/mL) Normal <15: Cardiac troponin (cTn) is the standard blood-based test to confirm the diagnosis of acute myocardial infarction. (See “Diagnosis of acute myocardial infarction”, section on ‘Definitions’.) However, troponin is not specific for acute thrombotic occlusion of a coronary artery, the most common precursor to acute myocardial infarction. Increased blood concentrations of cTn can also be seen in a variety of other diseases, such as sepsis, atrial fibrillation, heart failure, pulmonary embolism, myocarditis, myocardial contusion, and renal failure. In addition, stable chronic elevation of cardiac troponin may be detectable with high-sensitivity assays in patients with underlying structural (muscle) heart disease. Analytical false positives or false negatives are rare. https://www.uptodate.com/contents/elevated-cardiac-troponin-concentration-in-the-absence-of-an-acute-coronary-syndrome
- BNP (pg/mL) Normal <125: Brain natriuretic peptide, also called B-type natriuretic peptide (BNP), is a protein that the heart and blood vessels make. BNP helps the body eliminate fluids, relaxes blood vessels, and moves sodium into the urine. When the heart is damaged, the body secretes high levels of BNP into the bloodstream to try to ease the strain on the heart. One of the most important uses of BNP is to try to determine whether shortness of breath is due to heart failure. https://www.mayoclinic.org/diseases-conditions/heart-disease/in-depth/heart-disease/art-20049357
- CK (U/L) Normal <171: Creatine Kinase (CK), Total – Test for myocardial infarction and skeletal muscle damage. Elevated results may be due to myocarditis, myocardial infarction (heart attack), muscular dystrophy, muscle trauma, or excessive exercise. https://testdirectory.questdiagnostics.com/test/test-detail/374/creatine-kinase-ck-total?cc=MASTER
- CRP (mg/dL) Normal <0.5: CRP (C-reactive protein) is an acute-phase reactant protein that is primarily induced by the IL-6 (interleukin-6) action on the gene responsible for the transcription of CRP during the acute phase of an inflammatory/infectious process. https://www.ncbi.nlm.nih.gov/books/NBK441843/
Let’s wrap this up. It should be obvious that the Baumeier, et al. paper is very rich in details reflective of a best effort at a very high level.
We have looked at only one patient and now can go back an examine the remaining 14 that have more confounding variables such as pre-existing atherosclerotic heart disease.
Once you have completed the other 14, read the article to see if you agree with the conclusions. Are you convinced that BNT162b2 caused this very sick pump in an athletic young woman? If not, what happened to her?
Have you seen anything recently that looked like what happened to Patient 2, say on a football field?

How about sharing the medical findings since this was a public event and the public might benefit from understanding why young people are collapsing and dying suddenly?


Question: Kidney Issue >>> Heart Attack? What was the connection exactly between the kidney issue and massive heart attack?
Here is another example:


This is a necessary step to proper diagnosis and treatment of “vaccine”-harmed people.




I believe many post COVID patients without the injection may be experiencing the same but slower process of auto immune responses within their bodies. How can we help them reverse the response. Now the mRNA is in food and water. How do we protect the public? We get the vaccine killed some and will kill more but what those suffering from the COVID bio weapon? Can we help them? How?